Blood glucose meter purchasing advice: how to choose the right product
- What You Need to Know
- Glucose meters detect blood glucose levels.
- For the analysis, a small drop of blood is taken from the finger.
- So-called “continuous glucose meters” work without a needle.
- This level of control helps diabetics to cope with everyday life.
Glucose Meters: Control in Your Own Hands
Diabetes is a metabolic disease that affects more than 400 million people worldwide. It leads to high blood sugar levels. For proper treatment of the disease, it is necessary to regularly check blood sugar levels. This allows patients to take adequate measures when necessary. A glucose meter measures this value within a few seconds and stores the data. A physician can then use these values to adjust their treatment to the individual.
The term “blood sugar” describes the amount of glucose in blood. Cells in our body get their energy from glucose. The sugar contained in food quickly enters the bloodstream through the intestinal wall. Insulin is the hormone responsible for transporting glucose into cells where it is used. This means that insulin is important for lowering blood sugar levels. In diabetic patients, the body’s insulin production is altered, causing disturbances in blood sugar regulation.
Typical symptoms of diabetes include: increased urination, tiredness, poor concentration, problems with vision, occasional itching, severe thirst and cravings. Uncontrolled diabetes is dangerous because it can lead to other diseases. Diabetes increases the risk of developing high blood pressure and can also damage the eyes, nervous system, and heart.
It is very important that people with diabetes regularly monitor their blood sugar in order to treat the disease effectively. This monitoring can be carried out quickly and easily with a glucose meter. This device determines the concentration of glucose in a drop of blood. The blood is drawn with a small prick in the fingertip, applied to a test strip and evaluated by the meter.

Type 1 and Type 2 Diabetes
There are two known forms of diabetes, with type 2 being far more common than type 1. Type 1 diabetes is an autoimmune disease that often occurs at a young age. In those affected, the body’s own defenses destroy the insulin-producing beta cells in the pancreas. As a result, there is a lack of insulin, and the body no longer breaks down sugar properly. Insulin deficiency is a lifelong affliction, meaning that patients regularly have to inject insulin. The causes of type 1 diabetes remain unknown. Scientists suspect that the disease is genetic.
Type 2 diabetes is the most common type of diabetes. Here there is no insulin deficiency, but a kind of insulin resistance. Cells in the body respond poorly to the hormone, causing sugar to build up in the blood. In response, the pancreas increases the production of insulin. At some point the organ is so exhausted that insulin production declines. At this point an insulin deficiency sets in, which in many cases can only be compensated for by insulin injections.
Blood Sugar Levels
Sugar content in human blood changes depending on what has been consumed. To check blood sugar levels, it is essential to correctly interpret the displayed value on the meter. When specifying the value, confusion often arises because of different units of measurement:
- Millimoles per liter (mmol/l)
- Milligrams per deciliter (mg/dl)
Millimoles per liter indicates the number of sugar molecules per liter. It refers to the amount of a substance. Milligrams per deciliter, on the other hand, describe how much the sugar particles in one deciliter of blood weigh. This is a weight specification. Users should be aware of which unit their meter is displaying as both units are commonly found.
In order to recognise whether the displayed value is too high or too low, users need to know the standard values. A distinction is made between the value on an empty stomach (pre prandial), i.e., after eight to ten hours without food, and the value after eating (post prandial).
| Normal value in mg/dl | Normal value in mmol/L | |
| Pre Prandial | 60–100 mg/dl | 3.3–5.5 mmol/L |
| Post Prandial | 90–140 mg/dl | 5.0–7.8 mmol/L |
How Does a Glucose Meter Work?
Most measuring devices evaluate a blood sample, which is usually taken with a prick in the fingertip. Conventional glucose meters are smaller than a smartphone and can be carried around should they be needed. The meter includes a lancet, lancing device, and test strips. The lancet is a tiny steel blade with a plastic handle that is used to collect the blood sample. It can be inserted into a lancing device, which simplifies the puncture of the skin with the help of a spring mechanism. The drop of blood obtained is applied to a test strip, which the meter automatically evaluates.
What Kind of Glucose Meters Are Available?
There are two types of measuring device for use at home: the common sample method, or the insertion of sensors under the skin. The latest development is non-invasive equipment that uses infrared, although long-term studies of its reliability have yet to be conducted.
Invasive Sampling
Meters that measure from a blood sample are the most common. They can be used several times a day and require a very small amount of blood for chemical analysis. The blood sample is placed on a test strip and read by the meter. When used correctly, invasive spot-check meters provide the most reliable blood glucose readings.
There are two types of blood-sample glucose meter:
With single–use strip meters, users must use a new test strip each time they take a measurement. These meters are easy to use and small, but require you to carry accessories such as strips, lancets, and lancing devices.
Integrated glucose meters are a handy solution. The test strips are built into the device in the form of a cassette drum. The lancet is also part of the case. After installing the accessories, these meters are slightly larger than their competitors. Nevertheless, they are well suited for carrying around, as everything you need is at hand.

Invasive Measurement with Sensors (CGM)
CGM stands for “continuous glucose monitoring”. With this method, the meter automatically measures the glucose content in the tissue fluid of the fatty tissue under the skin. To achieve this, a small sensor with an insertion device is implanted under the skin. Users must change the sensor every 5 to 14 days. Alternatively, the sensor can be implanted by a healthcare professional and left under the skin for up to six months. The values recorded by the sensor are transferred directly to the connected meter. This enables the values to be observed in real time. The CGM is particularly useful for people who have to check their blood sugar levels frequently.
Non-Invasive Measurement
These devices represent the latest developments in glucose meters. They work without a blood sample or sensors. Instead, the finger is simply placed on an infrared sensor. Non-invasive measuring devices are still under development and there are no robust, long-term studies on reliability.
What to Look for When Buying a Blood Glucose Meter
There are a few factors that should determine your choice of a glucose meter. Mostly, they relate to suitability for everyday use. This is particularly important for people who have to measure their values frequently and want this to happen quickly and reliably.
Measurement Accuracy
A measuring device that gives inaccurate values is useless. The accuracy of the meter, therefore, is of utmost importance. In the EU, all blood sugar measuring devices must comply with ISO standard 15197:2015. It states that, if the blood sugar value is below 100 milligrams per deciliter (5.5 millimoles per liter), 95% of the measured values may be within a fluctuation range of plus or minus 15 milligrams per deciliter (1.8 millimoles per liter). If the blood sugar value is over 100 milligrams per deciliter, a deviation of no more than 15% is permitted.
Major manufacturers publish studies on the measurement accuracy of their devices. Details of these studies can be found in the package insert. The best solution is to have a doctor do a comparative measurement. This is the most reliable way of determining the precision of your device.
Operation and Display
A glucose meter should not complicate everyday life, rather it should make it easier. The simpler a meter is to operate, the easier it is for patients to use the equipment correctly and to avoid measurement errors. Easy-to-read, illuminating labels and pictograms help to make this easier. A glucose meter should have as large an illuminated display as possible so that the measurement data can be read clearly in all lighting conditions.
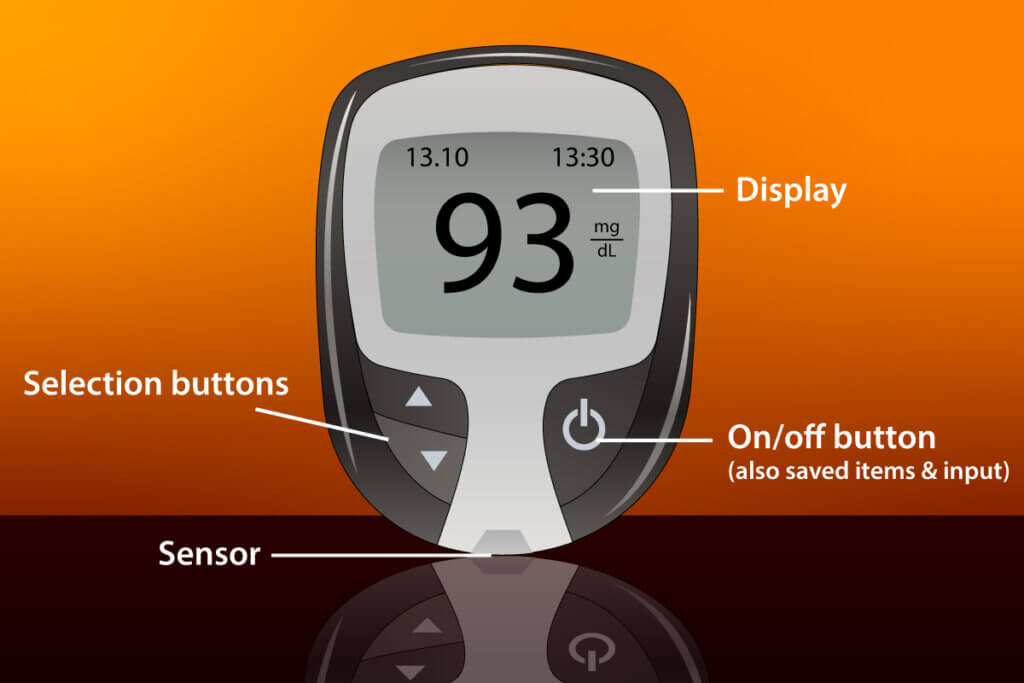
Most glucose meters have a similar design. The measurement result (or an error code in the event of an incorrect measurement) is displayed in the middle of the display. Above are the date and time. An apple stands for a measurement before a meal. An apple core symbolises a measurement after eating. A diary of recent values can be called up over the open book symbol. Meters usually have selection buttons and a confirmation button, which can also be used to switch the meter on and off.
Measurement Time
For many diabetics, the speed at which the meter can measure is important. A measuring device that delivers values quickly is more practical in everyday life. Most meters will display glucose levels a few seconds after inserting the test strip.
In the case of CGM devices, measuring time is less important than measuring frequency. The device determines the values at regular every-few-minute intervals and saves them automatically to be evaluated later on.
Size and Weight
These values have a large effect on the ease of everyday use. Based on these dimensions, you can work out how you would store a meter before making the decision to buy it. Most glucose meters are no bigger than a mobile phone and weigh between 30 and 50 grams. Although integrated glucose meters do not require any accessories, they are a little heavier.

Storage Space
Saving measurement results makes treating diabetes easier, as it allows the values to be analysed over a certain period of time. The size of the storage space is therefore important. A good measuring device should be able to store around 500 measurements.
A USB interface enables the data to be transferred to a computer or smartphone. This enables users to keep an electronic diabetes diary. Many manufacturers offer a free app for this.
Coding
Many current meters also have to be “coded”. This means adjusting the meter to new test strips. This is necessary to avoid deviations in the measurements. To do this, the code on the test strip pack must be entered in the meter.
Automatic coding makes using a meter easier, more time-efficient and safer. As soon as a test strip is inserted, the meter registers the new code. This eliminates the risk of forgetting a code or getting it wrong.
Extra Functions
These features go beyond the basic functions of a glucose meter. They are not strictly necessary, but can be useful and make a meter easier to use:
Many glucose meters have an alarm that reminds users to take a measurement.
With some meters it is possible to take blood samples not only from the fingertips, but from other parts of the body, such as the upper arm. This function is called “ATS”(alternative test sites).
A USB cable for data transfer is often included with a meter.
Some glucose meters even have wireless network or Bluetooth functions. Measurement results are transmitted wirelessly to a PC or smartphone.
Tips for Using a Glucose Meter
After a while, measuring blood sugar becomes a routine. To get started, it is helpful to remember a few tips. Lots of people also worry about whether the costs will be covered by their health insurance.
Sources of Measurement Error
In order to properly treat diabetes, it is essential that the measurement leads to accurate results. However, when using a glucose meter, there are some possible errors that can invalidate the result. Because of this, it is all the more important to first practice using the meter with a specialist.
A common mistake is to leave the jar containing the test strips open for too long, allowing moisture to get to the strips. It is better to always close the jar immediately after removing a strip.
It’s also important to note that a test strip becomes unusable if blood gets on it before it is inserted into the meter. Most models will not prompt users for a blood sample until the test strip has been properly inserted into the meter.
When collecting the drop of blood, do not prick the thumb or index finger, as these are the most commonly used fingers in everyday life. Many users take blood from the ring finger.
Avoid pricking the center of the fingertip, as it contains a lot of nerves. Instead, try to use the edge of the fingertip while regularly changing the finger.
Do not try to squeeze out a drop of blood. This causes cell fluid to escape, which can invalidate the measured value.
When applying the blood to the test strip, the finger must touch the side of the strip so that it absorbs the blood and transports it correctly to the measuring field. Do not hold your finger on the strip from above, as this prevents the blood from reaching the measurement area.
Recognising Errors
Many modern meters are error-sensitive, meaning that they recognise when the meter has been incorrectly used and display an error message instead of an incorrectly measured value. Depending on the model, the meter can specify exactly where the error occurred with clear text information.
What is covered on the NHS?
Anyone affected by type 1 or type 2 diabetes needs certain equipment for their treatment. Being insured on the NHS ensures that you have free access to diabetes treatment.
If you suffer from diabetes, you are entitled to free prescriptions for diabetes medicine. Free prescriptions can be claimed with the help of an exemption certificate, known as a “PF57 form”. This form can be applied for at your GP surgery and taken with you to the pharmacy when collecting prescriptions. You can even save your receipts from medicine bought before you receive your PF57 form and reclaim the money once you have it.
Improving Your Blood Sugar Levels
Nowadays, diabetes is a very treatable disease. As well as regularly self-monitoring and taking insulin, those affected also have other avenues for improving their health. Diet and exercise play an important role in the treatment of type 2 diabetes in particular. However, these tips are also helpful for patients with type 1 diabetes:
A balanced and healthy diet is essentially good for everyone. Overweight patients should try to reduce their weight slowly. Changing your eating habits is the most effective, long-term way of achieving this. Lots of fiber, fresh fruit, vegetables, and whole grain products make up a balanced diet.
Everyone, diabetics included, should make sure to drink enough fluids. At least 1.5 liters per day is recommended. Ideally, this should be water or other unsweetened drinks. If at all, diabetes patients should only drink alcohol on rare occasions.
Exercise is just as important. The aim is not to become a competitive athlete. Regular cycling, swimming, or even just going for a walk is sometimes enough. Small changes in habits can have a large effect. Leave the car and walk or climb the stairs instead of taking the lift.
Sleep disorders and lack of sleep have a negative effect on insulin release and blood sugar levels. It’s important that you get enough sleep. Also remember to take small breaks every day.
Smoking harms the body in many ways. It is believed that nicotine and other substances found in cigarettes have a harmful effect on insulin production.


















 2,858 reviews
2,858 reviews


